Results of a patient-led research project
Editor’s note: This is part two of a three-part series of articles from Dr. Kevin Austin, Adjunct Professor in the Health Futures Institute’s Personalized Medicine Centre at Murdoch University, Australia. He lives with IBM and turned his research skills toward a study to understand the priorities of those living with myositis and their care partners.
By Kevin Austin
In part 1 of this series, we revealed the priorities and challenges for Australian IBM patients, carers, and families. In this installment, we discuss how well they are coping (or not) with living and managing the risks and challenges they face on a day-to-day basis.
The 10 biggest challenges were, in order of importance, for patients and carers combined (details of what each heading meant can be found in the first blog of this series):
- Uncertain future: disease progression, housing needs, and loss of independence
- Coping with daily frustrations
- Lack of cure, treatment, and understanding
- Impact on carer’s capabilities and own needs
- Change of roles and relationships
- Getting information, education, and support when we need it
- Significant impact on our mental health
- Financial impact
- Issues with Australia’s disability and aged care systems
- Concern not covered by voluntary euthanasia
The following chart shows how well IBM patients and carers are coping (or not) with each of the significant challenges identified.
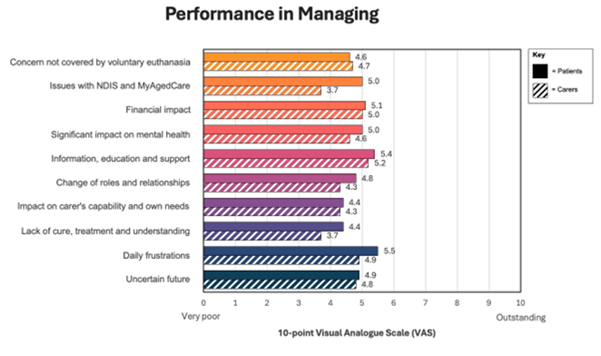
It can be seen that neither patients nor carers are coping well with any of the priority challenges. Overall, patients tend to cope a little better than carers. Carer burden is a significant priority. Additional analysis revealed that IBM patients and carers appeared to be coping less well than other forms of myositis.
Uncertainty has a direct impact on mental health
Life is tough just surviving on a day-to-day basis, particularly if one is living with IBM. Patients are really struggling with the day-to-day challenges in trying to merely get by and survive with the demands forced on them by living with IBM.
Even the most fundamental challenges are not addressed. Toileting, for example, can be a real challenge with the vast majority of public accessible toilets in Australia failing to meet the needs of myositis patients. A myositis patient is far more likely to suffer from urinary and fecal incontinence (shown in a recent different study), and the impact if away from home can be devastating. So getting out, going somewhere for a short break or holiday, meeting up with family and friends becomes a blocker or negative impact on mental health.
Sourcing of various pieces of equipment for different stages of severity of disease can also be really difficult and stressful.
Patients living in rural and remote regions find it even harder
Most participants reported frustration and difficulty in accessing medical specialists and allied health expertise, but this is even more challenging for those living in rural and remote regions. Some regional participants reported traveling over 12 hours for treatment.
Fear of living alone going into the future was often mentioned. Social issues were frequently mentioned (intimacy, sexuality, and relationship impact of myositis). Younger patients talked about their fears of not being around or loss of function and afraid of not being able to support their children growing up. We are planning to explore these themes and findings further and will be preparing subsequent publications to share this information.
Financial consequences can be severe
Financial burdens are real and faced by many living with myositis. There were many who reported financial difficulties in purchasing required supportive technologies and aids, for example, walkers, power wheelchairs, hospital style beds, toilet power raisers, etcetera.
Where can I go, what do I need now, versus what will I need in a year or two? Home and vehicle modifications can be exorbitant. Real concern of going bankrupt is on the rise, adding to an already significant mental health burden.
This adds to a general fear of financial inadequacy with dramatic increases in cost of living in Australia in recent times. It’s tough going. Patients are facing critical issues and challenges and are not managing or coping well with any of them.
One of our participants has recently been forced to surrender their car license. The sudden unexpected loss of independence has been quite profound.
Carers face their own challenges
Carers are facing critical issues and challenges and are also not coping or managing any of them particularly well. Poor management includes some of the most critical challenges. As the patients age, so do many of their carer/partners. Life is not only becoming tough for the patient, but the carer role is more difficult as well. Many of the study participants felt the role of carer was becoming more onerous.
There are some significant differences in perception of priorities between patients and carers. Several most important challenges to carers don’t appear to be acknowledged by patients. Carers find that the actual activity of caring has a significant impact on their “me” time. This appears to lead to a significant negative impact on their mental health. They are now unable to do many things they enjoyed doing before, largely due to their caring responsibilities.
There is a huge impact on relationships and, for couples, forced significant changes as carers go from loving relationships and lovers to being overwhelmed with just coping with added responsibilities of cooking, cleaning, administration, main breadwinner, and more.
Lack of an easy-to-understand disease framework
There doesn’t appear to be an easy-to-understand disease framework, so patients can’t figure out where they are in the IBM overall scheme of things and what might be coming next. Failure to understand is leading to increased anxiety around planning their future, downsizing their home, or obtaining equipment and assistive technologies.
Many differing opinions amongst the medical fraternity just add to the confusion, and carers struggle with where to go for quality help and support.
Through the eyes of patients and carers, their priorities are, perhaps, best summed up by a direct quote from an IBM patient that drew widespread support: “This disease sucks!”
Our final installment of this series will offer some initial ideas on how to better cope and improve resilience for those who live with IBM.

Thankyou for this information. I resonate with all of it.i am 62 years old and have been diagnosed with IBM 4 years ago. I have noticed significant progression in my abilities and am currently suffering with very low energy levels which doesn’t help when trying to maintain a regular exercise regime even though it is not at all strenuous by normal measures.i have been rejected by ndis twice which is upsetting. The reason for rejection was the proof of permanence of my condition. This is just so frustrating as there is no treatment or cure. I did include medical papers explaining my condition but this didn’t seem to make any difference. I’m finding it really hard to know who or how to get help from. I’m going back to my gp next week to start with my fatigue issues. Thanks again for your research I look forward to hearing and reading more. Paula Wilkins
Hi Paula, I’m 71 and diagnosed in 2019 with IBM. I’m currently a patient at Johns Hopkins and in their INSPIRE Research Program. I feel your frustration with the fatigue issues. It’s almost constant being tired. I’m told it’s just a fact of IBM life. It drives me nuts. Even just sitting or lying around I can feel fatigued. It’s the muscles wasting away. I’m now dependent on a Rollator more and more. I get my exercise at a Therapy Pool which is awesome because I have no fear of falling. Plus it feels so good to be able to move around. My best advice is to just try to carry on and keep moving. Hopefully they’ll be a future treatment of a cure. In the meantime hang in there and realize you’re not alone. Best of luck, John P. Lancaster, PA
Hi Paula
I am shocked to read that NDIS have rejected your applications as I have had their support for a number of years now and couldn’t manage without it. Please lodge an appeal and keep on trying before your age becomes a factor and they pass you on to the aged care system.
I am 64 and was diagnosed 5 years ago. Totally empathise with the issues you mention. Please give hydrotherapy a go if you can. It really helps physically and mentally
Thank you so much for this incredibly insightful research. I am 77 and was finally diagnosed 7 years ago. My husband is an absolute treasure but I feel for him as my condition deteriorates. He worries constantly about me falling. My levels of fatigue escalate as the day goes on, and sadly my patience and my thoughtfulness for my beautiful man go in the opposite direction. I couldn’t live at home without him and yet I can see how difficult it is for him every day. We have a wonderful 56 year strong marriage that’s worth taking good care of!